Since the 1950s, there have been drugs for treating depression, but not every drug works for every patient. Some patients do not need antidepressants, while others are resistant to all available medications.
At present, choosing the right drug for a person involves trial and error based on the effects of the drug. Using this method can lead to side effects and even worsen depression symptoms because it is very imprecise.
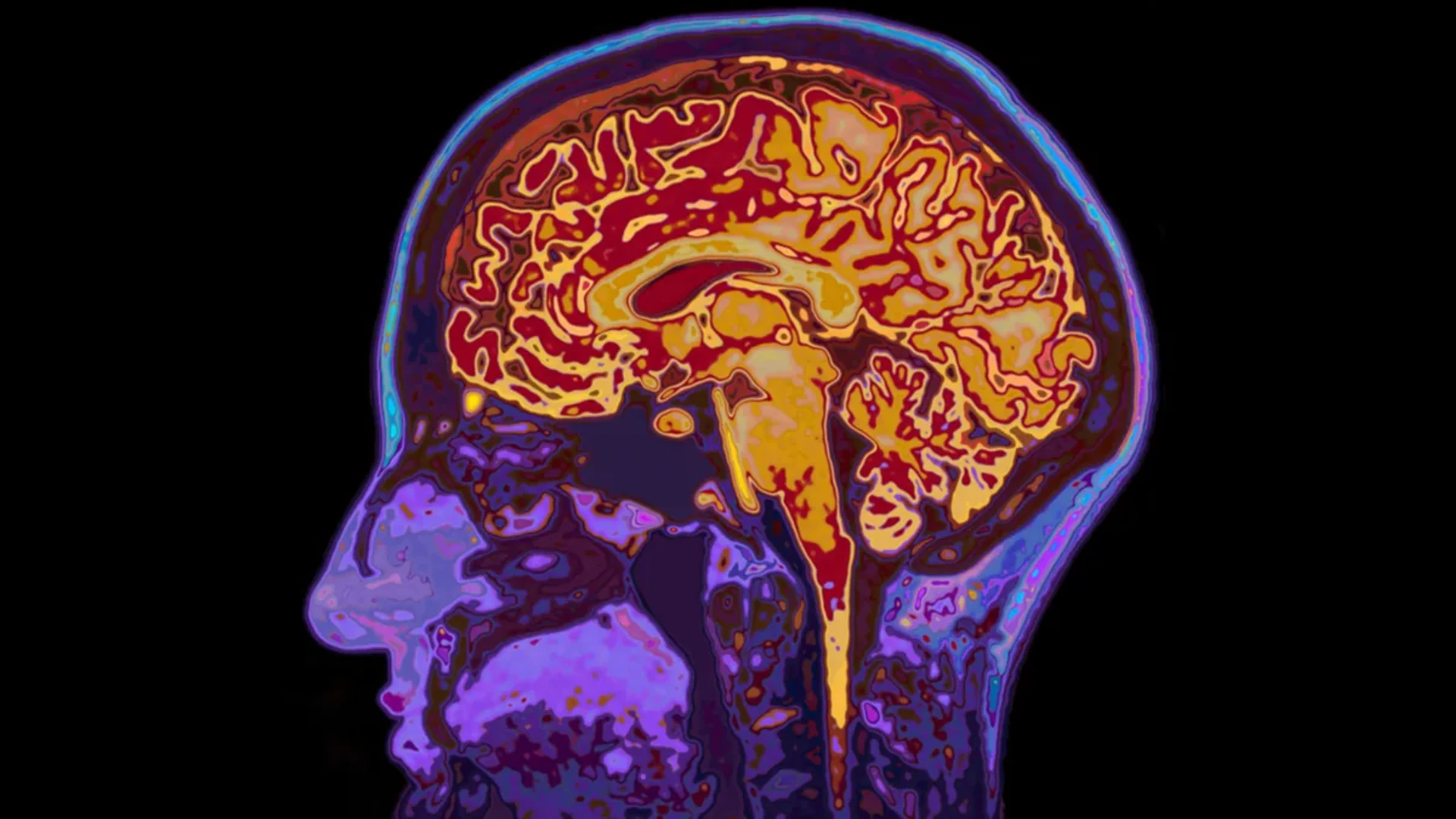
Now, Scientists at the Centre for Depression Research and Clinical Care, Peter O’Donnell Jr. Brain Institute have created a new technique of identifying if an anti-depressant is effective through imaging certain biomarkers in the brain.
In a paper released in the journal Biological Psychiatry, the researchers have discovered that a new method that is non-invasive may help to avoid patients experiencing from severe bouts of depression following consumption of the wrong medicine.
In this model, clinicians used machine learning techniques to look for specific changes in brain regions and their circuitry, which are typically associated with a response to medication.
Researchers used a common antidepressant drug and a placebo on a control group to test the method. Patients who did not respond to the original drug were switched to another.
“This is a significant advance. It’s non-invasive. It can be used immediately,” Madhukar Trivedi, professor of Clinical Psychiatry at the Peter O’Donnell Jr. Brain Institute, said in a Press Statement.
We measured the participants’ brain circuit changes using non-invasive functional magnetic resonance imaging (fMRI).
According to a press release, Albert Montillo, co-author of the paper and assistant professor at the Lyda Hill Department of Bioinformatics, “the signatures we found are unique to each antidepressant.”. Neuroscientists typically find that brain activity can explain 15% of the variance in symptom relief. That would be a significant finding. Twenty percent is big.”.